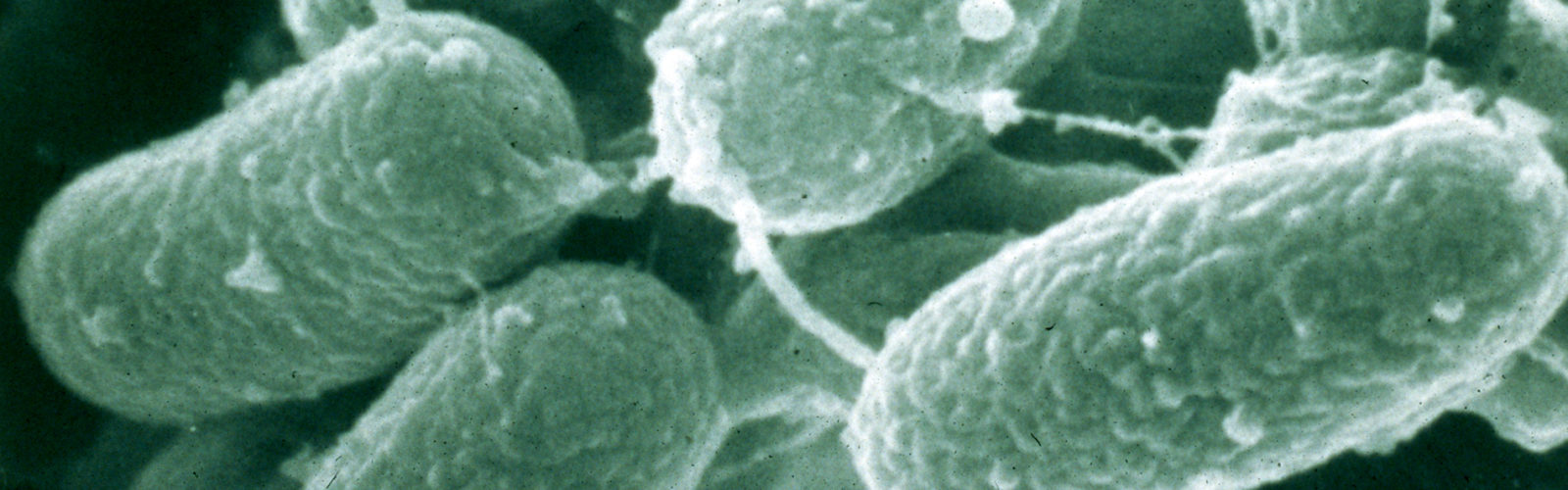
Raw food contamination by MAP
The majority of MAP infections occur in food-producing ruminants, i.e. cattle, goats and sheep. Meat and milk derived from MAP-infected animals is commonly contaminated before harvesting (slaughter), during the disseminated stage of MAP infections when the organism is found in muscle meat, internal organs, colostrum and milk, and the unborn fetus of pregnant animals. During harvesting of both milk and meat there is a second opportunity for MAP contamination of food products in conjunction with fecal contamination. Thus, raw products originating from herds or flocks of MAP-infected animals are likely to be MAP-contaminated. Counts up to 560 MAP/mL of raw milk from individual cows have been reported. The question then becomes whether manufacturing processes or cooking by the consumer will reliably kill MAP.
Pasteurized food products

The preponderance of work on the ability of food manufacturing processes to kill MAP has focused on pasteurization, specifically high-temperature short-time (HTST) pasteurization. Laboratory studies attempting to measure standard thermal tolerance parameters for MAP indicate that it is more heat-resistant than Mycobacterium bovis (the cause of bovine TB) and Coxiella burnetti (the cause of Q fever), the two milk-borne zoonotic pathogens designed to be killed by pasteurization. Corroborating this are multiple independent retail milk surveys reporting recovery of viable MAP by culture from retail HTST pasteurized milk. Clearly, HTST pasteurization kills large numbers of MAP in milk. However, evidence suggests that it does not kill 100% of MAP cells 100% of the time, or that post-pasteurization MAP contamination is frequently occurring. More details are provided under the topic MAP Biology/Resistance.
Cheese

High moisture, high pH, “fresh” (short time from production to consumption), cheeses made from raw milk have the greatest likelihood of containing MAP as well as other milk-borne bacterial pathogens like Listeria. However, MAP has been shown to persist even the processes involved in making low-moisture, low pH, aged cheese such as Swiss cheese, regardless of whether milk was first pasteurized or not.
Yogurt & other dairy products
MAP numbers in spiked yogurt were shown to persist during storage but decline somewhat in the presence of certain probiotic bacteria found in fermented milk products. Other dairy products such as ice cream or powdered milk preparations have not been studied.
Meat

The effect of cooking on MAP viability in meat has been studied far less than pasteurization. Empirically, if meat is cooked to a condition known as “well-done” (defined as when the meat juices run clear), then the center of the product has attained a core temperature equivalent to that of HTST pasteurization. Hence, one could predict low or no MAP recovery from well-done meat. This prediction is supported by two studies attempting recovery of MAP from naturally and intentionally contaminated meat. Meat not cooked until “well-done” could harbor viable MAP.
Ground beef represents the greatest potential risk for harboring MAP because:
- A significant proportion originates from culled dairy cattle which have the highest animal-level prevalence of MAP infections,
- Dairy cattle are culled when they are no longer productive and late stage MAP infections are a cause of low productivity,
- Fecal contamination of carcasses in the abattoir occurs, in spite of efforts to minimize it,
- Ground beef includes lymph nodes where MAP are concentrated, and
- The process of mixing and grinding beef to produce hamburger blends any MAP into the final product, away from the surface which is exposed to the highest level of heat during cooking. However, the frequency of finding viable MAP in retail meat has not been assessed. Arguably, E. coli O157 may serve as an indicator organism to gauge the frequency with which a zoonotic bacterial pathogen found in cattle feces contaminates ground beef. If one accepts this premise, then the frequent ground beef recalls due to E. coli O157 detection in the US suggests that MAP contamination of ground beef may be common. [see USDA site for product recalls and public health alerts]
Water
 Although not traditionally considered “food”, domestic water supplies must be considered in the context of food safety to insure a balanced perspective on potential modes of human exposure to MAP. Domestic water sources vary among and within communities. Tap water may originate from surface water, i.e. lakes and rivers, or underground, i.e. wells. Surface waters are generally a mix of rainwater runoff and artesian spring water. Rainwater falling on land occupied by MAP-infected cattle has the potential to harbor MAP and the organism will persist in rainwater runoff for a prolonged time, e.g. over a year. Mycobacteria, including MAP, are resistant to killing by the levels of chlorine commonly used to decontaminate domestic water. Hence, water may exposure humans to MAP either by drinking or by aerosolization and inhalation.
Although not traditionally considered “food”, domestic water supplies must be considered in the context of food safety to insure a balanced perspective on potential modes of human exposure to MAP. Domestic water sources vary among and within communities. Tap water may originate from surface water, i.e. lakes and rivers, or underground, i.e. wells. Surface waters are generally a mix of rainwater runoff and artesian spring water. Rainwater falling on land occupied by MAP-infected cattle has the potential to harbor MAP and the organism will persist in rainwater runoff for a prolonged time, e.g. over a year. Mycobacteria, including MAP, are resistant to killing by the levels of chlorine commonly used to decontaminate domestic water. Hence, water may exposure humans to MAP either by drinking or by aerosolization and inhalation.
Summary
Recent risk assessments concur in the conclusion that MAP contaminates raw products derived from MAP-infected animals and water runoff from MAP-infected farms, and that it may survive food manufacturing processes or cooking. The provocative discovery that MAP can produce spores [see Why so Resistant?] explains its persistence in the environment and its tenacity in the face of industrial processes designed to control food-borne bacterial pathogens. It remains to be proven what the real health consequences of MAP exposure or infection are for humans, and it will take considerable time and effort for medical science to resolve this question due, in part, to the chronic insidious nature of the diseases potentially involved and the lack of well standardized assays for MAP infection in humans.
Given the weight of evidence and the severity and magnitude of potential human health problems, the precautionary principle suggests that it is time to take actions to limit “as low as reasonably achievable” human exposure to MAP. All evidence suggests that the farm is the critical control point. Paratuberculosis control on farms serves to improve animal health and welfare, improve farm profitability, and lower MAP numbers in raw food products thereby lessening the likelihood and level of human exposure to MAP whether in dairy products, meat or domestic water supplies. With the rapid globalization of food production and trade, the challenge of MAP control for both animal health and consumer confidence in the safety of their food is international.
Reference List
- Alonso-Hearn M, Molina E, Geijo M, Vazquez P, Sevilla I, Garrido JM et al. Isolation of Mycobacterium avium subsp. paratuberculosis from muscle tissue of naturally infected cattle. Foodborne Pathogens and Disease 2009;6(4):513-518.
- Antognoli MC, Garry FB, Hirst HL, Lombard JE, Dennis MM, Gould DH et al. Characterization of Mycobacterium avium subspecies paratuberculosis dissemination in dairy cattle and its association with antemortem test results. Vet Microbiol 2008;127300-308.
- Ayele WY, Svastova P, Roubal P, Bartos M, Pavlik I. Mycobacterium avium subspecies paratuberculosis cultured from locally and commercially pasteurized cow’s milk in the Czech Republic. Appl Env Microbiol 2005;711210-1214.
- Beumer A, King D, Donohue M, Mistry J, Covert T, Pfaller S. Detection of Mycobacterium avium subsp. paratuberculosis in drinking water and biofilms by quantitative PCR. Appl Env Microbiol 2010;76(21):7367-7370.
- Botsaris G, Swift BMC, Slana I, Liapi M, Christodoulou M, Hatzitofi M, Christodoulou V, Rees CED. Detection of viable Mycobacterium avium subspecies paratuberculosis in
powdered infant formula by phage-PCR and confirmed by culture. International Journal of Food Microbiology 2016; 216:91–94. - Brady C, O’Grady D, O’Meara F, Egan J, Bassett H. Relationships between clinical signs, pathological changes and tissue distribution of Mycobacterium avium subspecies paratuberculosis in 21 cows from herds affected by Johne’s disease. Vet Rec 2008;162(5):147-152.
- Ellingson JLE, Anderson JL, Koziczkowski JJ, Radcliff RP, Sloan SJ, Allen SE et al. Detection of viable Mycobacterium avium subsp. paratuberculosis in retail pasteurized whole milk by two culture methods and PCR. J Food Prot 2005;67966-972.
- Eltholth MM, Marsh VR, Van Winden S, Guitian FJ. Contamination of food products with Mycobacterium avium paratuberculosis: a systematic review. J Appl Microbiol 2009;1071061-1071.
- Falkingham III JO. Nontuberculous mycobacteria from household plumbing of patients with nontuberculous mycobacteria disease. Emerging Infectious Diseases 2011;17(3):419-424.
- Gerrard ZE, Swift BMC, Botsaris G, Davidson RS, Hutchings MR, Huxley JN, Rees CED. Survival of Mycobacterium avium subspecies paratuberculosis in retail pasteurised milk. Food Microbiology 2018; 74: 57e63.
- Gill CO, Saucier L, Meadus WJ. Mycobacterium avium subsp. paratuberculosis in dairy products, meat, and drinking water. J Food Prot 2011;74(3):480-499.
- Grant IR. Mycobacterium avium subsp. paratuberculosis in animal-derived foods and the environment. In: Behr MA, Collins DM editors. Paratuberculosis – Organism, Disease, Control. Oxfordshire, UK: CABI, 2010, 29-39.
- Grant IR, Ball HJ, Rowe MT. Incidence of Mycobacterium paratuberculosis in bulk raw and commercially pasteurized cows’ milk from approved dairy processing establishments in the United Kingdom. Appl Env Microbiol 2002;682428-2435.
- Grant IR, Hitchings EI, McCartney A, Ferguson F, Rowe MT. Effect of commercial-scale high-temperature, short-time pasteurization on the viability of Mycobacterium paratuberculosis in naturally infected cows’ milk. Appl Env Microbiol 2002;68(2):602-607.
- Grant IR, Foddai ACG, Tarrant JC, Kunkel B, Hartmann FA, McGuirk S, Hansen C, Talaat AM, Collins MT. Viable Mycobacterium avium ssp. paratuberculosis isolated from calf milk replacer. J. Dairy Sci. 2017; 100:9723–9735.
- Le Dantec C, Duguet JP, Montiel A, Dumoutier N, Dubrou S, Vincent V. Chlorine disinfection of atypical mycobacteria isolated from a water distribution system. Appl Env Microbiol 2002;68(3):1025-1032.
- Mutharia LM, Klassen MD, Fairles J, Barbut S, Gill CO. Mycobacterium avium subsp. paratuberculosis in muscle, lymphatic and organ tissues from cows with advanced Johne’s disease. Int J Food Microbiol 2010;136(3):340-344.
- National Advisory Committee on Microbiological Criteria for Foods. Assessment of food as a source of exposure to Mycobacterium avium subspecies paratuberculosis (MAP). J Food Prot 2010;73(7):1357-1397.
- Pickup RW, Rhodes G, Arnott S, Sidi-Boumedine K, Bull TJ, Weightman A et al. Mycobacterium avium subspecies paratuberculosis in the catchment and water of the river Taff in South Wales, UK and its potential relationship to clustering of Crohn’s disease in the city of Cardiff. Appl Env Microbiol 2005;71(4):2130-2139.
- Peirce ES, Borowitz SM, Naser SA. The Broad Street pump revisited: dairy farms and
an ongoing outbreak of inflammatory bowel disease in Forest, Virginia. Gut Pathogens 2011; 3:20. - Pribylova R, Slana I, Kralik P, Kralova A, Babak V, Pavlik I. Correlation of Mycobacterium avium subsp. paratuberculosis counts in gastrointestinal tract, muscles of the diaphragm and the masseter of dairy cattle and potential risk for consumers. International Journal of Food Microbiology 2011; 151:314–318.
- Spahr U, Schafroth K. Fate of Mycobacterium avium subsp paratuberculosis in Swiss hard and semi-hard cheese manufactured from raw milk. Appl Env Microbiol 2001;67(9):4199-4205.
- Sung N, Collins MT. Thermal tolerance of Mycobacterium paratuberculosis. Appl Env Microbiol 1998;64999-1005.
- Sung N, Collins MT. Effect of three factors in cheese production (pH, salt, and heat) on Mycobacterium avium subsp paratuberculosis viability. Appl Env Microbiol 2000;66(4):1334-1339.
- Van Brandt L, Coudijzer K, Herman L, Michiels C, Hendrickx M, Vlaemynck G. Survival of Mycobacterium avium ssp. paratuberculosis in yoghurt and in commercial fermented milk products containing probiotic cultures. J Appl Microbiol 2011; 110:1252-1261.
- Whan LB, Grant IR, Ball HJ, Scott R, Rowe MT. Bactericidal effect of chlorine on Mycobacterium paratuberculosis in drinking water. Letters Appl Microbiol 2001;33(3):227-231.
- Whittington RJ, Waldron A, Warne D. Thermal inactivation profiles of Mycobacterium avium subsp. paratuberculosis in lamb skeletal muscle homogenate fluid. Int J Food Microbiol 2010; 137:32–39.
- Whittington RJ, Marsh IB, Reddacliff LA. Survival of Mycobacterium avium subsp. paratuberculosis in dam water and sediment. Appl Env Microbiol 2005;71(9):5304-5308.
- Williams AG, Withers SE. Microbiological characterisation of artisanal farmhouse cheeses manufactured in Scotland. International Journal of Dairy Technology 2010;63(3):356-369.