This is an accordion element with a series of buttons that open and close related content panels.
What causes Johne's disease?
Johne’s (pronounced “Yoh-nees”) disease and paratuberculosis are two names for the same animal disease. Named after a German veterinarian*, this fatal gastrointestinal disease was first clearly described in a dairy cow in 1895.
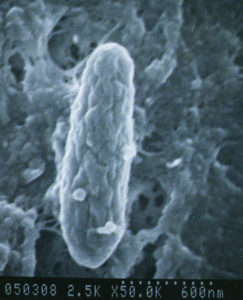
A bacterium named Mycobacterium avium subspecies paratuberculosis (let’s abbreviate that long name to “MAP”) causes Johne’s disease. The infection happens in the first few months of a calf ’s life but the animal may stay healthy for a very long time. Symptoms of disease may not show up for many months to years later. This infection is contagious, which means it can spread from one animal to another, and from one species to another (cows to goats, goats to sheep, etc.).
MAP is hardy – while it cannot replicate outside of an infected animal, it is resistant to heat, cold and drying. See “Biology of MAP” for more information about this bacterial pathogen.
(*Dr. Heinrich Albert Johne; follow the paths taken by scientists to understand Johne’s disease on the History page).
What kind of animals get Johne's disease?
Johne’s disease is primarily a health problem for ruminant species (ruminants are hoofed mammals that chew their cud and have a 3-4 chambered stomach) and occurs most frequently in domestic agriculture herds. Some of the more common ruminants are cattle, sheep, goats, deer, antelope, and bison. It is particularly common in dairy cattle, not because they are more susceptible to infection but because they are more frequently exposed to the organism that causes Johne’s disease (MAP). However, it is increasingly common among beef cattle herds, particularly those that trade animals frequently, such as breeders of purebred animals.
Infected ruminants have been reported from all parts of the world. Non-ruminants such as omnivores or carnivores (birds, raccoons, fox, mice, etc.) may become infected, but it is uncommon for them to become sick because of the infection.
What are the signs of Johne's disease in beef cattle and what causes them?
 There really are only two clinical signs of Johne’s disease in beef cattle: rapid weight loss and diarrhea. Of course, other diseases can cause similar clinical signs. The infection occurs in calves in the first months of life, but signs of disease usually do not appear until the animals are adults. Despite continuing to eat well, MAP-infected adult cows become emaciated and weak. Since the signs of Johne’s disease are similar to those for several other diseases, laboratory tests are needed to confirm a diagnosis. If a case of Johne’s disease occurs, it is very likely that other infected cows (who may still appear healthy) are in the herd.
There really are only two clinical signs of Johne’s disease in beef cattle: rapid weight loss and diarrhea. Of course, other diseases can cause similar clinical signs. The infection occurs in calves in the first months of life, but signs of disease usually do not appear until the animals are adults. Despite continuing to eat well, MAP-infected adult cows become emaciated and weak. Since the signs of Johne’s disease are similar to those for several other diseases, laboratory tests are needed to confirm a diagnosis. If a case of Johne’s disease occurs, it is very likely that other infected cows (who may still appear healthy) are in the herd.
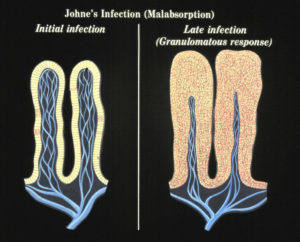
The granulomatous inflammation leads to intestinal thickening and malabsorption as evidenced by diarrhea and weight loss. No one yet understands what causes a clinically normal cow that has been infected by MAP for months or years to suddenly become sick from the infection. We do know that at some point the MAP that have been lying quiet within cells of the last section of the small intestine (called the ileum) start to replicate and take over more and more of the tissue. The bovine immune system responds to all these organisms with what is called granulomatous inflammation. This inflammation thickens the intestinal wall, preventing it from functioning normally. This, among other factors, means the cow cannot absorb the nutrition it needs and thus begins to lose body condition, milk production drops off, and diarrhea may occur. In effect, an animal with Johne’s disease is starving in spite of having a good appetite and eating well.
 Sometimes, the malnutrition induced by the MAP infection causes low serum protein levels. Serum proteins help animals retain fluid within blood vessels, called oncotic pressure. When serum protein levels get too low, fluid leaks out into the surrounding tissues. In cattle, this is seen as submandibular edema – more commonly called “bottle jaw”, as in the Waygu cow pictured to the left.
Sometimes, the malnutrition induced by the MAP infection causes low serum protein levels. Serum proteins help animals retain fluid within blood vessels, called oncotic pressure. When serum protein levels get too low, fluid leaks out into the surrounding tissues. In cattle, this is seen as submandibular edema – more commonly called “bottle jaw”, as in the Waygu cow pictured to the left.
How common is Johne's disease in beef cattle?
 In 1997 the USDA conducted the first and only survey of U.S. beef cattle herds using a commercially available blood test (ELISA). They tested 10,372 cows in 380 herds finding that 7.9% of herds had 1 or more ELISA-positive cows. They also discovered that 92% of beef producers were either unaware of Johne’s disease or recognized the name but knew little about it. Also worth noting about that survey is that 70% of surveyed herds were commercial cow-calf operations (average herd size 137 cows). The remainder were registered (purebred) herds or herds with a combination of both commercial and registered cattle.
In 1997 the USDA conducted the first and only survey of U.S. beef cattle herds using a commercially available blood test (ELISA). They tested 10,372 cows in 380 herds finding that 7.9% of herds had 1 or more ELISA-positive cows. They also discovered that 92% of beef producers were either unaware of Johne’s disease or recognized the name but knew little about it. Also worth noting about that survey is that 70% of surveyed herds were commercial cow-calf operations (average herd size 137 cows). The remainder were registered (purebred) herds or herds with a combination of both commercial and registered cattle.
Data from the Johne’s Testing Center (JTC) suggest that Johne’s disease is much more common. In 2017 the JTC found that 18% of 578 fecal samples submitted from beef cattle were PCR-positive for MAP (Randall et al, 2018 AABP proceedings). Granted, this is not a survey: These samples most often were submitted because of a suspicion of Johne’s disease. However, most of these samples came from registered (purebred) beef cattle herds of many different breeds from across the U.S. These findings and the impressions of veterinary practitioners indicate that Johne’s disease is far more common in beef cattle, particularly herds with registered cattle, than most people realize.
Prevalence studies in Europe, summarized by Nielsen & Toft (Prev.Vet.Med. 88:1-14,2009) reported MAP infection prevalence in cattle but did not discriminate between dairy cattle and beef cattle. In Europe many cattle are dual purpose, i.e. used for both dairy and beef production.
Ho do beef cattle get infected?
 Johne’s disease typically enters a herd of animals when a MAP-infected, but healthy-looking, animal is purchased. This infected animal then sheds MAP bacteria onto the premises – perhaps onto pasture or into water shared by its new herdmates. Contaminated ponds, low-lying areas on farms that trap rainwater, are are particular concern as they catch pasture runoff and become a “poop-soup” where MAP bacteria can persist.
Johne’s disease typically enters a herd of animals when a MAP-infected, but healthy-looking, animal is purchased. This infected animal then sheds MAP bacteria onto the premises – perhaps onto pasture or into water shared by its new herdmates. Contaminated ponds, low-lying areas on farms that trap rainwater, are are particular concern as they catch pasture runoff and become a “poop-soup” where MAP bacteria can persist.
 Young animals are far more susceptible to infection than are adults: these calves swallow the organism along MAP-contaminated milk, water or feed. Often, MAP-contaminated milk is collected from the infected but healthy-appearing animals. The milk may become contaminated from the environment (manure-stained teats) or, in the advanced stages of the infection, the bacterium is shed directly into the milk. Animals may even have been infected before they are born (called in utero transmission). Thus the infection spreads, often without the owner’s being aware of it.
Young animals are far more susceptible to infection than are adults: these calves swallow the organism along MAP-contaminated milk, water or feed. Often, MAP-contaminated milk is collected from the infected but healthy-appearing animals. The milk may become contaminated from the environment (manure-stained teats) or, in the advanced stages of the infection, the bacterium is shed directly into the milk. Animals may even have been infected before they are born (called in utero transmission). Thus the infection spreads, often without the owner’s being aware of it.
How can you prevent your herd from becoming infected?
 Do not introduce it with purchased or leased animals! Try to purchase animals from a source herd free of Johne’s disease, based on whole-herd testing. Second best is to work with producer who knows the level of Johne’s disease in his or her herd and follows good infection control practices. Then, purchase test-negative animals from test-negative dams. Remember that Johne’s disease is a herd problem, and that knowing the test-status of numerous adults in the source herd will give you a much better sense of the risk of purchasing an infected animal than the one test result you might get on the one animal you wish to buy. Evaluating a source herd is not always easy but keeping the infection out of your herd is much less costly and troublesome than controlling it once it gets in. Laboratory tests are available for all animal species – you can even test fecal material collected from the environment nowadays.
Do not introduce it with purchased or leased animals! Try to purchase animals from a source herd free of Johne’s disease, based on whole-herd testing. Second best is to work with producer who knows the level of Johne’s disease in his or her herd and follows good infection control practices. Then, purchase test-negative animals from test-negative dams. Remember that Johne’s disease is a herd problem, and that knowing the test-status of numerous adults in the source herd will give you a much better sense of the risk of purchasing an infected animal than the one test result you might get on the one animal you wish to buy. Evaluating a source herd is not always easy but keeping the infection out of your herd is much less costly and troublesome than controlling it once it gets in. Laboratory tests are available for all animal species – you can even test fecal material collected from the environment nowadays.
How can you test cattle for Johne's disease?
New approaches are now available for testing that are cheaper and more reliable than ever before. There are two basic testing strategies: 1) detect MAP bacteria in fecal samples, or 2) detect an immune response (antibodies) to MAP using blood samples. Detecting MAP directly is the more accurate, but also a more expensive, diagnostic method. MAP can be rapidly detected by a technology called PCR. Alternatively culture-methods can be used to grow MAP from fecal samples, a process taking 2-3 months. PCR and culture are equally accurate.
The serum portion of blood samples samples are used to detect antibodies to MAP using technology called ELISA. There are several commercial ELISA kits for Johne’s disease. ELISAs have much lower diagnostic sensitivity (ability to detect MAP-infected animals) compared to methods for detecting MAP bacteria in fecal samples. ELISAs typically have a diagnostic specificity of roughly 99.5%, meaning false-positive results can occur, but infrequently. For this reason, ELISAs are considered “screening tests” and under most circumstances should be followed up with a confirmatory test, i.e. MAP detection test. The lower cost of ELISAs makes them a popular test.
 MAP detection methods can be done on “pooled” samples. This involves submission of fecal samples from individual animals. The laboratory then mixes equal amounts of feces from 5 animals and then does a single test on that pool. If the pool is test-positive, then the fecal samples used for that pool are tested individually. This can significantly decreasing the cost per animal tested in a herd but is only appropriate for herds that are either not MAP-infected (surveillance testing) or are infected at a low prevalence (percentage of animals infected in the herd or flock).
MAP detection methods can be done on “pooled” samples. This involves submission of fecal samples from individual animals. The laboratory then mixes equal amounts of feces from 5 animals and then does a single test on that pool. If the pool is test-positive, then the fecal samples used for that pool are tested individually. This can significantly decreasing the cost per animal tested in a herd but is only appropriate for herds that are either not MAP-infected (surveillance testing) or are infected at a low prevalence (percentage of animals infected in the herd or flock).
More details on diagnostic testing can be found by selecting an beef cattle in the menu bar and then topic “Diagnosis” on the right-hand menu. Consult with your veterinarian to select the best approach for your animals and situation. You can also select “Testing Services” in the menu bar to be directly connected to the Johne’s disease testing information provided by the Wisconsin Veterinary Diagnostic Laboratory.
Ho do you control Johne's disease?
 The best methods for MAP infection control in your herd depend on the resources available, the goals of your enterprise, and the methods you use to take care of your cows. All control methods however rely on two core strategies that must be employed at the same time:
The best methods for MAP infection control in your herd depend on the resources available, the goals of your enterprise, and the methods you use to take care of your cows. All control methods however rely on two core strategies that must be employed at the same time:
- Calves must be protected from infection by being born and raised in a clean environment. The primary sources of MAP contamination are manure and/or milk from an infected adult animal. Moving the cow-calf pair out of the calving area s soon as possible limits exposure of calves to manure from other potentially MAP-infected cows and lessens the chances for cross-nursing.
- Adult animals infected with MAP must be identified and culled or at least kept out of the primary calving area to ensure no calves are exposed to their milk or manure.
These recommendations are consistent with the Sandhills Calving System, methods designed to protect calves from scours and other infectious diseases. The Sandhills Calving System uses larger, contiguous, pastures for calving, rather than high animal-density calving lots. Readers are encouraged to follow this link for more information.
Can Johne's disease be cured?
No. In the few studies that attempted to treat Johne’s disease with antibiotics, symptoms appeared to subside but animals relapsed after therapy was halted. As with other mycobacterial infections (for instance, human tuberculosis) multiple antibiotics must be injected or given orally daily for months. For most animals, this is cost-prohibitive as well as not feasible because the required drugs are not legal for use in food-producing animals.
Can humans get Johne's disease?
The term “Johne’s disease” is used only to describe the clinical illness in ruminants that occurs after MAP infection.
There is a human ailment however called “Crohn’s disease” that in many ways resembles Johne’s disease. Crohn’s disease is a chronic inflammatory bowel disease (IBD) that has no proven cause and no known cure. The consensus of several studies is that MAP is consistently “associated” with Crohn’s disease patients as compared to controls. Whether that association is causal or coincidental remains unknown. Some researchers believe MAP is the cause of Crohn’s disease for at least a subset of patients and multiple reports describe clinical improvement of Crohn’s disease patients using anti-MAP antibiotics. The majority of gastroenterologists, however, believe that MAP, if found in patients, is simply a by-stander amongst the many other organisms that are found in an inflamed, malfunctioning gastrointestinal tract. No connection has been shown between contact with animals having Johne’s disease or dairy product consumption and Crohn’s disease. This aspect of MAP is a complex and controversial area of scientific investigation.
A detailed discussion of this topic can be found in “Zoonotic Potential” on this website.

