PROPHETIC WORDS FROM 1922
2020-05-23 18:24:25Ninety-eight years ago today, two University of Wisconsin faculty published a seminal article on Johne’s disease. The full article is provided here for Johne’s history enthusiasts. Although published so long ago, the descriptions of the pathology and epidemiology of the disease are remarkably accurate. The tile page is shown below. Today’s Johne’s news highlights some of the prophetic statements made by those authors.
Beach and Hastings said:
“Johne’s disease is one that is not at all widespread in Wisconsin or in any part of our country at present. It does occur, however, and as the years go by it will become more and more common and will place a greater tax on the cattle industry unless some consideration is given to it by those engaged in the raising and sale of cattle.”
“The affected animals lose flesh very slowly until they become virtually walking skeletons. The unthrifty condition of animals, in spite of abundant feed, is occasioned in part by this disease.”
“…it is likely to be present in pure bred herds from which animals are being sold in great numbers. A few such distributing centers will thus spread with a constantly increasing rapidity unless more attention is paid too it that is done at present.”
“The aim of this bulletin is to call the attention of veterinarians and breeders to Johne’s disease, which, it is felt, is not recognized by many, in order that steps may be taken to prevent its introduction into still healthy herds, and to gradually eliminate it from affected herds.”

 These statements were published by B.A. Beach and E.G. Hastings in 1922 in the Wisconsin Bulletin, a publication by the Wisconsin Agriculture Experiment Station. Their warnings remain true today and their aim, to raise awareness, is the same aim as that of this website.
These statements were published by B.A. Beach and E.G. Hastings in 1922 in the Wisconsin Bulletin, a publication by the Wisconsin Agriculture Experiment Station. Their warnings remain true today and their aim, to raise awareness, is the same aim as that of this website.
Fast forward 98 years and, based on USDA survey data from 2007, we find that over 90% of U.S. dairy herds are now MAP-infected (Lombard et al., 2013), and the situation in most other major dairy-producing countries is similar. Millions of animals have died or been culled from herds due to this disease. Millions of dollars in farm income are lost annually because we failed to heed these warnings. And, we now find the cause of Johne’s disease, MAP, affecting beef cattle, sheep, goats, bison, as well as wild animals and spilling into humans through contaminated food and water. A tragedy that could have been averted.
MODELS FOR JD STUDY
2020-05-15 17:27:29 Dr. Judy Stabel, from the U.S. National Animal Disease Center, and colleagues have published a study comparing three animals, calves, lambs, and baby goats for the study of paratuberculosis following experimental challenge. Their research publication will appear in the July 2020 (volume 225) issue of the journal Veterinary Immunology and Immunopathology.
Dr. Judy Stabel, from the U.S. National Animal Disease Center, and colleagues have published a study comparing three animals, calves, lambs, and baby goats for the study of paratuberculosis following experimental challenge. Their research publication will appear in the July 2020 (volume 225) issue of the journal Veterinary Immunology and Immunopathology.
Abstract
Animal infection models to study Mycobacterium avium subsp. paratuberculosis (MAP) infection are useful for evaluating the efficacy of vaccines and other therapeutics for the prevention or treatment of infection. The goal of the present study was to compare smaller ruminants, sheep and goats, with calves as infection models. Neonatal sheep, goats, and calves (n = 4) received 109 cfu of a cattle isolate of MAP in milk replacer on days 0, 3 and 6 in a 12-month study and sampled monthly thereafter. Results demonstrated a robust antigen-specific IFN-γ response at 90 days post-inoculation for sheep and goats, with lower responses noted for calves. By 360 days, IFN-γ responses were 50 and 82% higher for calves than for goats and sheep, respectively. Although MAP-specific antibody responses were first observed in sheep at 90 days, calves had higher antibody responses throughout the remainder of the study. Following pass-through shedding on day 7, fecal shedding was fairly negligible across treatments but remained higher for calves throughout the study. Colonization of tissues was variable within treatment group and was higher for calves and sheep for the majority of tissues. Upon antigen stimulation of PBMCs, higher populations of CD4 + T cells cells and lower populations of γδ TCR + and NK cells were observed for goats and calves compared to sheep. Relative gene expression of IL-4, IL-12, and IL-17 in PBMCs was higher in goats, corresponding to lower tissue colonization with MAP. These data suggest that ruminant species are fairly comparable as infection models for MAP, but discrete differences in host responses to MAP infection exist between species.
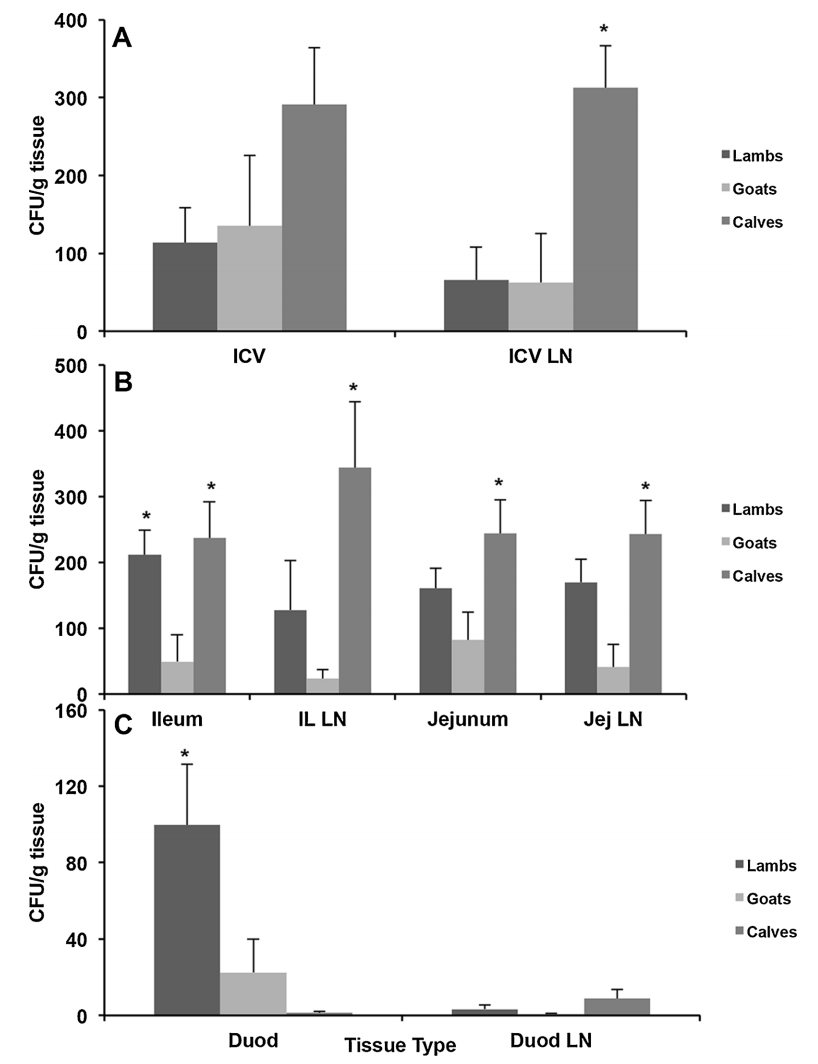
Summary (from article)
In summary, although sheep and goats share many similar properties as infection models to calves, overall calves proved to be a more standardized model with demonstrable fecal shedding, tissue colonization and host immune responses upon long-term infection. It is certainly up to the researcher to define their needs and goals in order to select the appropriate infection model. This may be impacted by practical factors associated with housing and feeding of animals in long-term studies as well as being driven by producer interest in the dominant livestock species in the region.
JD COMMON IN BRAZILIAN BUFFALO
2020-05-08 21:04:33 H. de Mores Pereira from the State University of Maranhão, São Luís, MA, Brazil and seven colleagues describe the high prevalence of subclinical paratuberculosis in Buffaloes (Bubalus bubalis) in a northeast region of Brazil. Their publication appears in the Brazilian Journal of Microbiology (published 14 April 2020). According to Wikipedia, Buffaloes are extensively used there for meat and dairy production. In 2005, the water buffalo herd in the Brazilian Amazon stood at roughly 1.6 million head, of which 460,000 were located in the lower Amazon floodplains.
H. de Mores Pereira from the State University of Maranhão, São Luís, MA, Brazil and seven colleagues describe the high prevalence of subclinical paratuberculosis in Buffaloes (Bubalus bubalis) in a northeast region of Brazil. Their publication appears in the Brazilian Journal of Microbiology (published 14 April 2020). According to Wikipedia, Buffaloes are extensively used there for meat and dairy production. In 2005, the water buffalo herd in the Brazilian Amazon stood at roughly 1.6 million head, of which 460,000 were located in the lower Amazon floodplains.

Photo credit: By Kleomarlo - Own work, CC BY-SA 3.0
Abstract
Paratuberculosis is an infectious, chronic, and incurable disease that affects ruminants, causing enteritis and chronic granulomatous lymphadenitis, characterized by malabsorption syndrome, its agent is the Mycobacterium avium subsp. paratuberculosis (MAP). Thus, the objective of this work was to identify and characterize MAP in buffalo herds slaughtered in Baixada Maranhense region. Samples of intestines, mesenteric lymph nodes, and ileocecal valves were collected from 115 buffaloes slaughtered at Baixada Maranhense slaughterhouses to perform the diagnosis by histopathological examination using staining with Hematoxylin and Eosin (H&E) and Ziehl-Neelsen, bacterial isolation, and real-time PCR. In the histopathology by H&E staining, there was evidence suggestive of paratuberculosis in 30% (31/115) of the buffaloes. With Ziehl-Neelsen staining, acid-fast bacilli (AFB) were visualized in 27% (26/115) of the tissue samples analyzed. MAP was isolated in 4.3% (5/115) of the fecal samples subjected to bacterial culture. The samples inoculated in HEYM with mycobactin J produced colonies identified with MAP according to their own morphological characteristics such as round, white, smooth and slightly rough, alcohol-acid staining, and slow growth with 8 weeks of incubation and mycobactin dependence. The agent confirmation was performed in five bacterial isolates (4.3%) and 15 (13%) fragments of jejunum, ileum, and mesenteric lymph node by the IS900 real-time PCR technique. The results of the present study demonstrate the subclinical occurrence of paratuberculosis in flocks of buffalo slaughtered in slaughterhouses of Baixada Maranhense.
JOHNE’S IN EUROPE: 2010-2017
2020-05-02 17:07:54Angela Fanelli, from the Department of Veterinary Sciences, University of Turin, Italy and three colleagues review the paratuberculosis situation in Europe from 2010 to 2017 using reports submitted to the O.I.E. (World Organization for Animal Health). Their report (8 pages with 30 references) appears in Veterinaria Italiana (56(1):13-21, 2020).
Summary
Mycobacterium avium subsp. paratuberculosis (MAP) is the etiological agent of paratuberculosis (PTB), a disease affecting domestic and wild ruminants. MAP may also play a zoonotic role in Crohn’s disease. Although both governments and industries are carrying out programmes to prevent and control the infection, there is a lack of harmonization across Europe. Moreover, the success of these programmes is influenced by the current lack of sensitivity of the diagnostic tests used. For these reasons, it is complex to evaluate the overall epidemiological situation of this disease. This study describes the European distribution of PTB from 2010 to 2017 using the information reported by Member Countries to the OIE. Countries were classified in three categories (‘Absent’, ‘Epizootic’, ‘Enzootic’) depending on the disease epidemiology, and the trend of countries reporting the disease presence was computed throughout the study period. A multilevel model with random slope was built for twelve countries, with complete reporting history. Most of the countries (57.44%) were classified as ‘Enzootic’. The percentage of countries reporting the disease presence slightly increased along the study period, probably due to the improvement of PTB monitoring, rather than to a deterioration of the epidemiological situation of the disease in Europe. Results of the model account for different dynamics in the number of outbreaks reported by ‘Enzootic’ and ‘Epizootic’ countries.
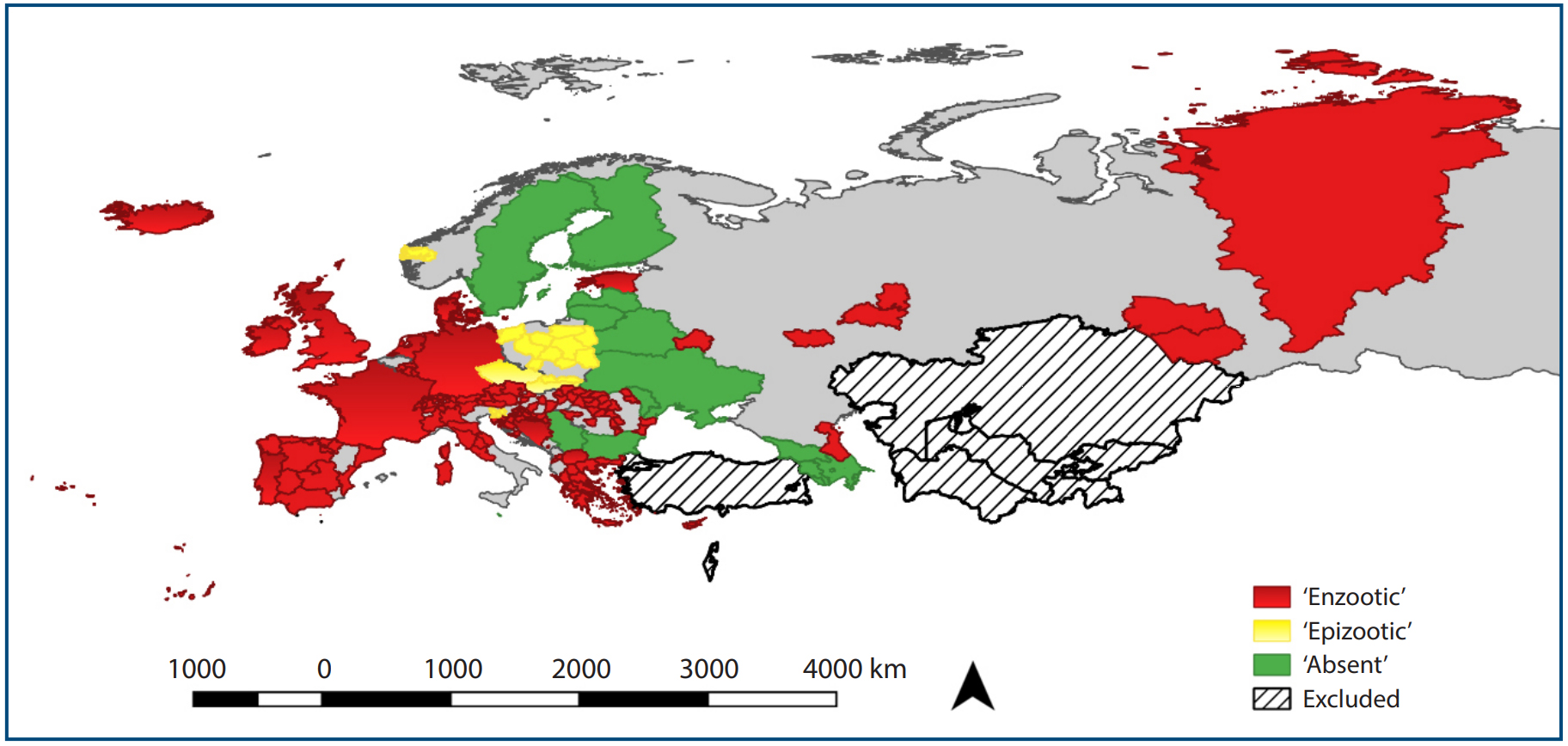
Conclusions
MAP infection leads to economic losses in farms. The bacteria may also have a role in the development of Crohn’s disease in humans. For these reasons, PTB control has arisen interest of countries over time. The restriction of livestock and dairy marketing in case of infection imposed by some countries has globally led to develop more efficient surveillance programmes. Despite these attempts, there is still a wide variation both in MAP reporting and monitoring among countries. This is the first study describing the epidemiological situation of PTB at regional scale using data of the OIE reporting system (WAHIS). The different levels of reporting of the epidemiological situation of the disease, mainly for what concerns quantitative information (no constant quality of information provided by all the countries along the period of study), may bias some of our results. Despite this, the main strength of the study is that it takes into consideration only information reported by veterinary services at the OIE, and represents so the most complete officially reported situation of the disease in Europe. This is also one of the few epidemiological studies implementing a multilevel model to describe heterogeneous data on the number of outbreaks reported. The results presented must be carefully interpreted in the light of the disease epidemiology and different level of surveillance. For a better control of the disease, countries should improve their monitoring systems, in order to increase surveillance and probability of outbreaks detection in both domestic animals and wild species. This study will serve as a basis for further studies on the epidemiological status of PTB at regional scale.
Comment: As the authors noted in their conclusions, reporting accuracy to O.I.E. (World Organization for Animal Health) is imperfect. Anecdotally, some political entities have suppressed reporting of paratuberculosis in the past. For another perspective on the global paratuberculosis situation the recent report by Whittington et al. is highly recommended.
ASK AND EXPERT – EDITORIAL
2020-04-24 16:34:55The “Ask and Expert” feature of this website receives several questions from animal owners and veterinarians each week. Questions from owners of pet goats are among the most common. Pet goats (companion animals) are most often Nigerian Dwarf goats and American Pygmy goats. These animals are cute, cuddly and have a marvelous personality.

The questions the website receives obviously concern Johne’s disease. Today’s news item highlights several general observations from these submitted questions:
- Pet goat owners, unlike cattle ranchers and dairy farmers, need more advice and help regarding infectious diseases such as Johne’s disease that are common in animal agriculture.
- Goat owners find it difficult to get veterinary services. There seem to be three reasons for this. First, veterinarians who work with large, food-producing animals such as dairy cattle and are most knowledgeable and experienced in working with Johne’s disease, typically do not work with companion animals like these small goats. Second, small animal veterinarians who work with pets like dogs and cats are unfamiliar with goats and their diseases. Lastly, goat owners are typically hobbyists who do not always fully appreciate the need for, and cost of, veterinary services.
- A last generalization from Ask and Expert questions is that pet goat owners, just like farmers and ranchers, need to practice better biosecurity to prevent their animals from becoming infected with this chronic, contagious, incurable disease known as Johne’s disease. Like other animal breeders, they trade animals among their small “club” without first asking for laboratory evidence that the source “herd” is free of MAP. The consequence is that the infection readily spreads with heart-breaking consequences.
It is my hope that this news item stimulates veterinarians who traditionally work with large or small animals to welcome pet goat owners as clients and become better informed about their special needs, and for pet goat owners to seek out such veterinarians interested in pet goats for the health and welfare of the animals they love so much.
For more information please see our website pages devoted to goats: https://johnes.org/goats/faqs/
This research article from our research team is one of the few specifically concerning Johne’s disease in pygmy and dwarf goats: Manning, E.J.B., Steinberg, H., Krebs, V., and Collins, M.T. 2003. Diagnostic testing patterns of natural Mycobacterium paratuberculosis infection in pygmy goats. Canadian Journal of Veterinary Research 67:213-218.

PROFOUND CD REMISSION
2020-04-17 16:19:24Crohn’s disease has been considered an incurable disease of unknown etiology. Today’s news posting is about yet another research article, published April 9, 2020, that challenges this prevailing opinion: Agrawal et al. Profound remission of Crohn’s disease requiring no further treatment for 3-23 years: a case series. Gut Pathogens (2020) 12:16. [OPEN ACCESS]
Abstract
Background: Crohn’s disease (CD) is rising in incidence and has a high morbidity and increased mortality. Current treatment use immunosuppressives but efficacy is sub-optimal, and relapse is common. It has been shown that there is an imbalance present in the gut microbiome (dysbiosis) in CD with a possible infective aetiology—Mycobacterium avium subsp. paratuberculosis (MAP) being the most proposed. Antibacterial therapy and Faecal Microbiota Transplantation (FMT) are emerging treatments which can result in clinical and endoscopic remission, if employed correctly. The objective of this study was to report on the treatment and clinical outcomes of patients with CD in prolonged remission.
Results: Ten patients were identified to have achieved prolonged remission for 3–23 years (median 8.5 years). Of these, 7/10 took targeted Anti-MAP therapy (AMAT) for a median 36 months and then ceased AMAT treatment. After stopping AMAT five patients underwent Faecal Microbiota Transplantation (FMT) (average four infusions). In 4/7, AMAT was combined with infiximab (mean of six infusions) that was withdrawn within 6 months after fistulae resolution. One patient achieved deep mucosal healing with AMAT alone. Of the 3/10 patients not prescribed AMAT, one had a combination of anti-inflammatory agents and a single antibiotic (metronidazole) followed by FMT. The other two received only FMT for Clostridioides difficile Infection.
Conclusions: Prolonged remission has been achieved for 3–23 years with individualised treatments, with the majority using AMAT ± infiximab and FMT. Treatment with antibiotics and/or FMT provides a potential new avenue for treatment of CD. These findings should stimulate thinking, investigations and better therapy against MAP and the dysbiosis of the gut fora, to enable higher rates of prolonged remission.
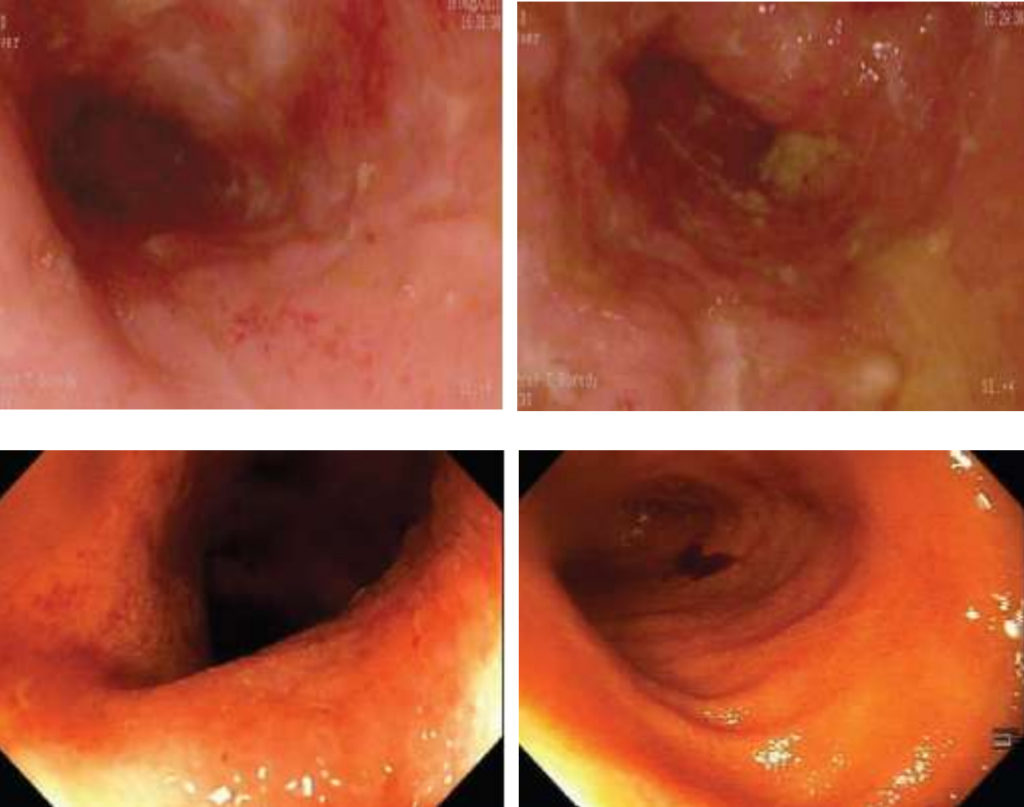
These endocsopy images from before and after treatment from Dr. Agrawal's article offer convincing evidence.
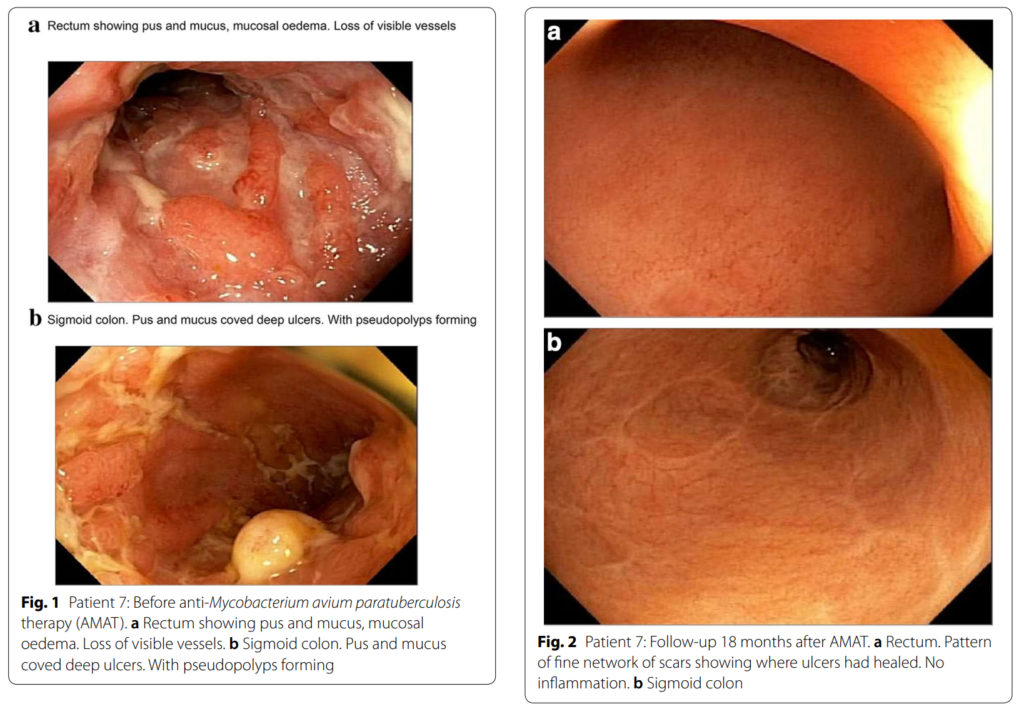
Comment: Here’s a short list of published findings implicating MAP, the accepted cause of Johne’s disease (JD), as a cause of Crohn’s disease (CD):
- JD and CD are clinically similar.
- JD and CD share similar histopathology.
- All slow growing mycobacteria are zoonotic.
- The incidence of CD has been rising for decades; a pattern suggestive of an infectious disease.
- MAP is found by culture or PCR in CD patients more often than controls.
- CD patients have antibody to MAP more often than controls.
- CD patients have cell-mediated immune responses (CD4-reactive T-cells) to MAP more often than controls.
- Explants of human fetal intestine in SCID mice have been experimentally infected with MAP proving the gut of humans is susceptible to MAP infection.
- Treatment of CD with anti-MAP antibiotics shows significant clinical and endoscopic improvement of patients (RedHill trial) as well in the recent case series by Agrawal in this and prior news postings.
- Countries with the highest prevalence of CD are also countries with the highest prevalence of animals with JD.
- There are many ways humans are being exposed daily to MAP through food and water.
Closing Observation:
MAP is a zoonotic infectious disease that has spilled over from animals to humans, just like COVID-19. It is not recognized as such for many reasons, one being antiquated ideas, and another being that its spread is measured in decades, not days. It is a stealthy pathogen that society must reckon with.
Concern for public health is just one of many reasons Johne’s disease must be controlled in animals.
CHRONIC INFECTION – SUDDEN CLINICAL ONSET
2020-04-10 16:40:54True story from the field highlighting the chronic nature of MAP-infections and the rapid onset of clinical signs.
 Shown here is a Dorper sheep (a fast-growing meat-producing sheep breed) born April 2015 in the U.S. In June of 2019, as part of a whole-flock test for Johne's disease using pooled fecal PCR, this animal tested PCR-positive. The PCR Ct value was 25 indicating high levels of MAP shedding in feces (estimated at 10,000,000 MAP per gram of feces). And yet this ewe which was 4-years-old at the time of testing, was clinically normal, as seen in the photo to the right taken just 60 days before the clinical signs began (age 4.9 years). It should be noted that this ewe produced son that was a grand champion and one of the more valuable animals in the flock. So, she was placed in isolation on the ranch.
Shown here is a Dorper sheep (a fast-growing meat-producing sheep breed) born April 2015 in the U.S. In June of 2019, as part of a whole-flock test for Johne's disease using pooled fecal PCR, this animal tested PCR-positive. The PCR Ct value was 25 indicating high levels of MAP shedding in feces (estimated at 10,000,000 MAP per gram of feces). And yet this ewe which was 4-years-old at the time of testing, was clinically normal, as seen in the photo to the right taken just 60 days before the clinical signs began (age 4.9 years). It should be noted that this ewe produced son that was a grand champion and one of the more valuable animals in the flock. So, she was placed in isolation on the ranch.
 By April of 2020 (10 months after testing PCR-positive) this ewe was showing clinical signs of Johne's disease. The rapid decline in body condition occurred in a matter of a few weeks. The next two images show her side-view and rear-view.
By April of 2020 (10 months after testing PCR-positive) this ewe was showing clinical signs of Johne's disease. The rapid decline in body condition occurred in a matter of a few weeks. The next two images show her side-view and rear-view.
 This series of slides illustrates the insidious nature of Johne's disease. It silently enters sheep flocks with purchased animals, it slowly spreads to lambs in the flock. Scientific consensus is that most animal become MAP-infected soon after birth. The incubation period (period from infection to clinical signs) is long – in this animal at least 4 years. Even when the infection is fairly advanced and the sheep is shedding millions of MAP per gram of feces, the animal looks in perfect health. However, inevitably the animal develops clinical signs of Johne's disease, weight loss and pasty feces.
This series of slides illustrates the insidious nature of Johne's disease. It silently enters sheep flocks with purchased animals, it slowly spreads to lambs in the flock. Scientific consensus is that most animal become MAP-infected soon after birth. The incubation period (period from infection to clinical signs) is long – in this animal at least 4 years. Even when the infection is fairly advanced and the sheep is shedding millions of MAP per gram of feces, the animal looks in perfect health. However, inevitably the animal develops clinical signs of Johne's disease, weight loss and pasty feces.
Although the animal has been MAP-infected for most of its life, the onset of clinical disease is sudden. Owners can mistakenly assume that the MAP-infection was recent when in fact the animal was infected for most of its life and shedding massive numbers of MAP capable of infecting lambs born on the property. This is why the infection is so insidious and why routine whole flock (or herd) testing using the most sensitive diagnostic test (PCR) is critical for effective control of Johne’s disease.
Side note: This problem occurred in a registered breeding flock with excellent animal husbandry and nutrition. In less well-managed flocks clinical signs may have appeared earlier.
Lessons:
- To avoid this problem, pre-purchase testing of the flocks you intend to buy from is vital.
- To diagnose the problem early before too many sheep are infected, annual whole-flock testing by fecal PCR is essential.
- Johne's disease is a major risk to elite breeding sheep flocks and can force a loss of valuable genetics. This makes Johne's disease an industry-wide problem that every breeder should tackle.
For more images of sheep with clinical paratuberculosis, visit this page of our website.
We are grateful for the information and photos provided by the flock owners for this story.
IS MAP ZOONOTIC? – WHAT DO VETS SAY?
2020-04-03 15:04:47Research Article
 Australia is a global leader in Johne’s disease control. They have developed control programs for a range of ruminant species and done some of the finest epidemiological research. They were the first to develop an ELISA kit for Johne’s disease, among many other firsts in the science of paratuberculosis.
Australia is a global leader in Johne’s disease control. They have developed control programs for a range of ruminant species and done some of the finest epidemiological research. They were the first to develop an ELISA kit for Johne’s disease, among many other firsts in the science of paratuberculosis.
Not surprisingly, Australia is now the first to systematically assess the perceptions of veterinarians regarding the zoonotic potential of MAP. This study was reported by members of the Sydney School of Veterinary Science, Faculty of Science, The University of Sydney in the Open Access journal Veterinary Sciences. They found that almost one-third of the respondents (32.2%) considered that MAP was likely to be involved in the causation of Crohn’s disease whereas more than two-thirds (69.8%) agreed with the adoption of the precautionary principle against Johne’s disease.
Abstract
Public concerns over exposure to Mycobacterium avium subspecies paratuberculosis (MAP) or MAP components via foods of animal origin could have negative trade consequences, despite the absence of conclusive scientific evidence of a causal association between MAP and Crohn’s disease (CD).
This study was conducted among Australian veterinarians to understand (a) their perceptions regarding the role of MAP in the causation of CD (an ordinal outcome), and (b) their consideration of the adoption of the precautionary principle against Johne’s disease (JD; a binary outcome). Ordinal and binary logistic regression analyses were performed to evaluate the association of explanatory variables with the above outcomes, respectively.
Almost one-third of the respondents (32.2%) considered that MAP was likely to be involved in the causation of CD whereas more than two-thirds (69.8%) agreed with the adoption of the precautionary principle against JD. Veterinarians who were concerned about exposure to and/or getting infected with MAP were more likely to consider MAP as a causative agent of CD (odds ratio: 7.63; 95% CI: 1.55, 37.63) and favor the adoption of the precautionary principle against JD (odds ratio: 6.20; 95% CI: 1.90, 20.25). Those perceiving MAP as a causative agent of CD were also more likely to favor the adoption of the precautionary principle against JD (odds ratio: 13.2; 95% CI: 1.26, 138.90).
The results suggest that Australian veterinarians, particularly those who consider MAP as a causative agent of CD are concerned about exposure to MAP and favor the adoption of the precautionary principle against JD. These findings can be useful for animal health authorities for designing JD control programs and policies.
Comments: This is the first formal survey of veterinary practitioners regarding the MAP zoonosis question. The article does an exceptional job of analyzing the data and underlying associations. Such as year of graduation, gender, and prior diagnosis of JD, related to veterinary opinions. I urge you to read the full Open Access article.
RAPID ID OF MAP BY MALDI-TOF
2020-03-27 14:44:21Research Poster
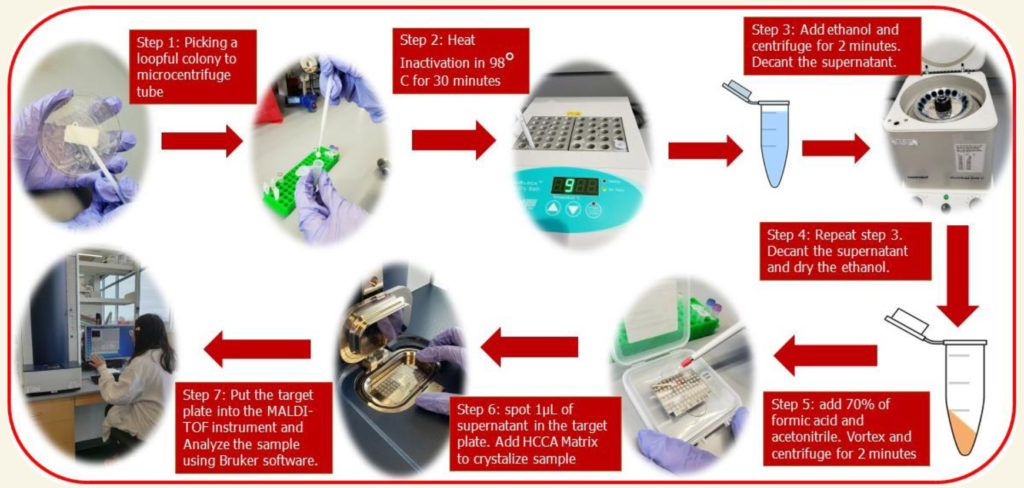
Undergraduate student, Claudia Antonika, at the University of Nebraska-Lincoln, under the direction of Dr. John D. Loy, in the School of Veterinary Medicine and Biomedical Sciences, evaluated the ability of the Matrix Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI-ToF) to distinguish Mycobacterium avium subspecies paratuberculosis (MAP) from other members of the Mycobacterium Avium Complex (MAC), such as Mycobacterium avium subspecies hominissuis (MAH) and Mycobacterium avium subspecies avium (MAA) using the Bruker Biotyper MAlDI-ToF instrument (pictured below) and software. This research was presented as a poster at the University of Nebraska and is available here.

Results: MALDI spectral profiles evaluated by the Bruker Daltonics (BDAL) database only classified 20% (9/45) of M. avium subspecies correctly. In contrast, when the spectral patterns were matched against a new main consensus library (MSP database), 84% (38/45) of M. avium were accurately identified at the subspecies level, including 93% (26/28) MAP.
Conclusions: MALDI-ToF can improve the ability of labs to rapidly identify multiple M. avium subspecies. The new library database created in this project significantly enhances the specificity of the instrument as it increases the matching score values. Kappa analysis showed good strength agreement. Over 84% of the isolates could be classified correctly using our new MSP database, whereas current database BDAL only could identify 20% of MAC isolates. Although there were seven isolates that failed to have higher score values when using our MSP database, their top match values were still greater as compared to BDAL database score. Therefore, we consider that our new MSP database is a large improvement over the previous database.
Credits: This Poster is brought to you for free and open access by the UCARE: Undergraduate Creative Activities & Research Experiences at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in UCARE Research Products by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln.
Comment: This is the largest study of MAP identification using MALDI-ToF, the current standard for bacterial identification in clinical microbiology laboratories. It provides an improved database with which to compare new M. avium isolates greatly improving identification accuracy. Moreover, it provides a new method for MAP identification that is independent of the genetics of MAP isolates, i.e. does not use genetic targets such as IS900 or HspX, to identify this M. avium subspecies. The only other main genetic-independent methods are: 1) exceptionally slow growth and 2) in vitro dependence on mycobactin for growth.
GOOD NEWS FOR CROHN’S
2020-03-20 14:00:32Research Article
 In prior clinical trials, all patients treated with anti-mycobacterial antibiotic therapy (AMAT) had been on standard anti-inflammatory drugs before being referred for AMAT, i.e. AMAT as second-line therapy. A new study by G. Agrawal from the Centre for Digestive Diseases, New South Wales, Australia (Prof. Thomas Borody, Director) reported for the first time a case series (8 patients) of treatment-naïve Crohn’s Disease patients treated with AMAT as first-line therapy. This OPEN ACCESS article was published March 6, 2020 in the journal Microorganisms, volume 8 issue 3 page 371.
In prior clinical trials, all patients treated with anti-mycobacterial antibiotic therapy (AMAT) had been on standard anti-inflammatory drugs before being referred for AMAT, i.e. AMAT as second-line therapy. A new study by G. Agrawal from the Centre for Digestive Diseases, New South Wales, Australia (Prof. Thomas Borody, Director) reported for the first time a case series (8 patients) of treatment-naïve Crohn’s Disease patients treated with AMAT as first-line therapy. This OPEN ACCESS article was published March 6, 2020 in the journal Microorganisms, volume 8 issue 3 page 371.
Abstract
Prospective trials of anti-mycobacterial antibiotic therapy (AMAT) have proven efficacious in Crohn’s disease (CD) but use as first-line treatment in CD has not been evaluated. This paper reports the outcomes of patients with CD treated with first-line AMAT. This paper consists of a case series of treatment-naïve CD patients who received AMAT as first-line treatment between 2007 and 2014 at a single center. AMAT treatment consisted of rifabutin, clofazimine and clarithromycin, plus either ciprofloxacin, metronidazole or ethambutol. Symptoms, inflammatory blood markers, colonoscopy and histology results, in addition to, the Crohn’s Disease Activity Index (CDAI) were tabulated from patients’ clinical records, and descriptive statistics were conducted. A Wilcoxon signed-rank test assessed the difference in CDAI scores before and while on AMAT. The statistical significance was set at 5%.
Clinical remission (CDAI < 150) with rapid improvement in clinical symptoms and inflammatory markers was seen in all eight patients receiving AMAT as sole therapy by 6 weeks. In all eight patients, the median CDAI score decreased significantly, from 289 prior to treatment to 62 at the 12-month follow-up (p < 0.001). Follow-up colonoscopies showed healing of CD ulcers, no visible mucosal inflammation, restoration of normal vascular patterns and complete mucosal healing on histology samples. AMAT as first-line therapy demonstrated a rapid improvement of Crohn’s disease (not previously seen when used as second-line therapy).
Author’s Conclusion
Our results dictate that future trials also examine AMAT as a first-line rather than rescue therapy. In addition, a four-drug combination is thought to be optimal, and AMAT’s decreased side effect profile and omission of immune suppression therapy make it a favorable option for a future pediatric study.
Comments: This case series adds further support to the hypothesis that MAP is a zoonotic pathogen and a cause of Crohn’s disease. It also gives hope to people suffering from this chronic debilitating disease.
« Previous 1 … 8 9 10 11 12 … 18 Next »